Vivir con esclerosis múltiple (EM) conlleva desafíos únicos, y tomar las riendas de nuestra vida puede significar algo diferente para cada persona. Las personas que tienen un sentido de control sobre su vida son más propensas a asumir responsabilidad y a hacer los cambios necesarios para gestionar mejor su bienestar. Por otro lado, si creemos que las cosas están completamente fuera de nuestro alcance, es posible que tengamos menos motivación para hacer cambios saludables. Aunque la EM puede ser impredecible, hay muchas maneras de recuperar y mantener un sentido de control sobre nuestras vidas y asumir una actitud proactiva sobre nuestra salud.
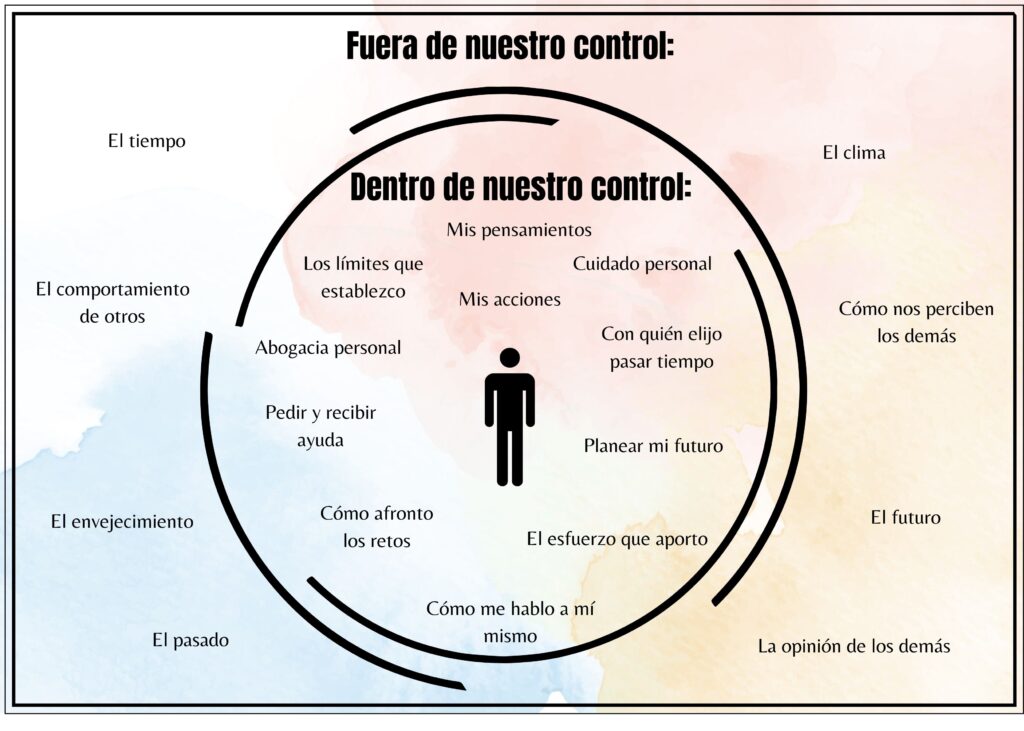
Es fundamental reconocer que existe una diferencia entre lo que está dentro y fuera de nuestro control. Aunque podemos influir en nuestros pensamientos, emociones y comportamientos, no siempre podemos controlar nuestro cuerpo, a los demás, el tiempo o nuestro entorno. La siguiente ilustración representa las cosas que normalmente están bajo nuestro control y algunas que pueden estar fuera de nuestro alcance.
Entre las cosas que están bajo nuestro control se incluyen:
- Nuestros pensamientos y emociones: La EM puede influir negativamente en nuestros sentimientos y en las decisiones que tomamos. Alguien que se siente en control puede tomar decisiones más saludables como salir a pasear o tomarse un tiempo para descansar, a otros les puede resultar más difícil hacer los cambios necesarios para controlar sus síntomas. Existe una gran variedad de herramientas, técnicas y recursos que pueden ayudarnos a manejar los retos emocionales. La psicoterapia puede ayudar a las personas con una amplia variedad de trastornos psicológicos y dificultades emocionales. Puede enseñarnos nuevas herramientas para afrontar los retos con mayor eficacia.
- Autocuidado – Ser una prioridad es vital para nuestro bienestar. Asegure dedicarse algo de tiempo, aunque esté muy ocupado. Puede consistir en hacer una pausa de 15 minutos sin interrupciones para tomar un café y utilizar ese tiempo para estar consigo mismo. Tómese un momento para enfocarse en su estado físico, mental y emocional. El autocuidado puede ser diferente para cada persona; puede ser tan sencillo como darse permiso para decir “no” a algo que no quiere hacer.
- Abogacía personal – Abogar por nosotros mismos es importante en la toma de decisiones compartidas. Conozca sus derechos, haga preguntas, pida una explicación en términos sencillos que pueda entender, tenga sus preguntas preparadas para sus citas médicas, infórmese sobre las opciones de tratamiento, manténgase al día con las últimas investigaciones y no tema pedir una segunda opinión. Mantener un registro de sus síntomas y efectos secundarios y discutirlo con su médico puede facilitar el proceso. La aplicación móvil gratuita de la MSAA, My MS Manager™ Mobile App ofrece una herramienta conveniente y eficaz para manejar el curso cambiante de esta enfermedad (disponible solo en ingles).
- Elija con quién pasa el tiempo – Elija pasar tiempo con quienes le apoyan, aquellos que intentan comprender sus necesidades y respetan sus experiencias únicas. Mantenerse social puede variar según sus preferencias y necesidades de salud. Permítase tiempo para descansar y reprograme las salidas cuando sea necesario. La comunicación con sus seres queridos es clave. Aproveche al máximo el momento en que se sienta mejor para programar actividades sociales; a veces los planes espontáneos son los más divertidos.
- El esfuerzo que hacemos/ nuestras acciones – El compromiso y el esfuerzo que invertimos en nuestros objetivos está a nuestro alcance. Podemos probar nuevas recetas o alimentos más saludables, explorar opciones de ejercicio para encontrar una rutina que funcione bien para nosotros o simplemente enfocarnos en reducir la frecuencia con la que nos damos ciertos gustos. Los cambios pequeños pueden hacer la diferencia.
- Cómo nos hablamos a nosotros mismos – La forma en que nos hablamos puede ser beneficiosa o dañina. A menudo olvidamos lo importante que es ser amables con nosotros mismos y cómo esto puede repercutir en otros aspectos de nuestras vidas. El diálogo interno negativo puede contribuir a la duda y la desesperanza. En cambio, el diálogo interno positivo puede promover sentimientos de empoderamiento a la hora de tomar decisiones sobre nuestra salud.
- Nuestra disposición a pedir y recibir ayuda – Reconocer cuándo necesitamos ayuda y estar dispuestos a recibir esa ayuda es muy importante. Puede ser difícil admitir que necesitamos ayuda, pero buscar recursos y apoyo puede ser sencillo. Considere la posibilidad de acudir a un grupo de apoyo, llamar a un amigo o familiar que le comprenda, o llamar a una línea de ayuda. Pedir ayuda puede ser el primer paso más valiente que pueda dar. No tiene por qué hacerlo solo; todos nos necesitamos.
- Los límites que establecemos – Establecer límites sanos y respetarlos requiere práctica. No basta con establecer límites; debemos respetarlos y ser constantes. Establecer un límite suena a: “No me siento cómodo con eso, si sigues haciéndolo me iré”. No puede controlar lo que hacen los demás, pero puede controlar su respuesta.
Puede que no tengamos control sobre ciertas cosas como lo que piensan los demás, el clima y la respuesta de nuestro cuerpo a ciertos tratamientos, pero sí tenemos el poder de dar forma a nuestra propia historia a partir de ahora. Es natural sentir frustración o desesperanza cuando nos enfrentamos a cosas que no podemos controlar, pero siempre hay una opción. Tenemos el poder de tomar decisiones sobre nuestros cuerpos, decisiones médicas y estilos de vida. Cada día es una oportunidad nueva para invertir en nosotros mismos.
¿Qué significa para usted tomar el control de su vida y de su salud? ¿Tiene algún consejo o técnica que le haya ayudado a retomar el control y manejar su bienestar?